is metamucil good for diabetics
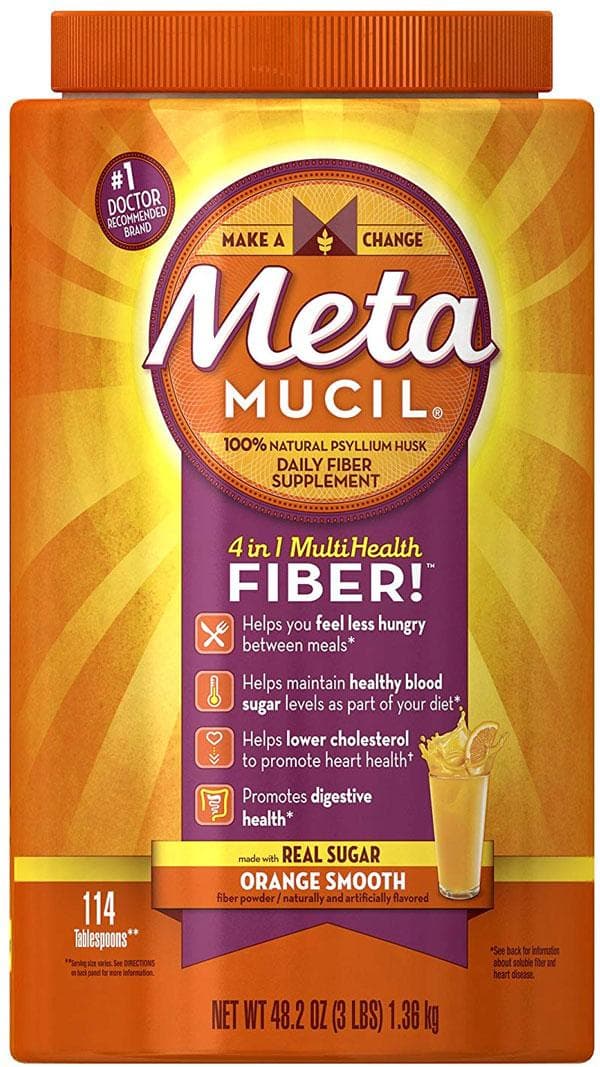
Article Contents Effects of glucose psyllium and serum lipid responses in men with type 2 diabetes and hypercholesterolemia CiteJames W Anderson, Lisa D Allgood, Jan Turner, Peter R Oeltgen, Bruce P Daggy, psyllium effects on glucose and responses of serum lipids in men with type 2 diabetes and hypercholesterolemia, The American Journal of Clinical Nutrition, Volume 70, Issue 4, October 1999, Pages 466–473, ABSTRACTBackground: Postndial concentrations decreases This study examined the effects of psyllium management for men with type 2 diabetes. Objective: The objective was to assess the safety and effectiveness of the psyllium shell fiber used in conjunction with a traditional diabetes diet in the treatment of men with type 2 diabetes and mild to moderate hypercholesterolemia. Design: After a dietary stabilization phase of 2 kwk, 34 men with type 2 diabetes and mild to moderate hypercholesterolemia were randomly assigned to receive 5.1 g psyllium or cellulose placebo twice a day for 8 wk. Biweekly lipid and blood glucemic indexes were evaluated on an outpatient basis and weeks 0 and 8 in a metabolic pavilion. Results: In the metabolic pavilion, the psyllium group showed significant improvements in glucose and lipid values compared to the placebo group. Total concentrations of serum and LDL cholesterol were 8.9 per cent (P Conclusion: The addition of psyllium to a traditional diet for people with diabetes is safe, well tolerated and improves glucemic and lipid control in men with type 2 diabetes and hypercholesterolemia. INTRODUCTIONThe sillium shell fiber is a viscose fiber, mainly soluble in water prepared by the mechanical removal of the skin of the blonde psyllium seed (Plantago ovata). Early or uncontrolled studies suggest that the psyllium improved glucemic and lipid control in individuals with type 2 diabetes (–). Although a more recent and carefully controlled study reported a decrease in postprandial glucose and insulin concentrations with the supplementation of psyllium in type 2 diabetes (), other studies found no effect on glucemic control () or an effect only when the psyllium was sprayed or incorporated into a cereal meal (). It has been shown that piss significantly reduces postprandial serum glucose and insulin concentrations in non-diabetic individuals (). Numerous studies of non-diabetic individuals indicate that psyllium significantly decreases both total concentrations and LDL-cholesterol (–). However, the safety and effectiveness of the psyllium has not been well documented for people with type 2 diabetes and hypercholesterolemia. Diabetes' control and complications test convincingly showed that maintaining good glucemic control slowed the appearance and slowed the evolution of complications in individuals with type 1 diabetes. Many healthy individuals with type 2 diabetes can also benefit from better glucemic control (). In addition, type 2 diabetes dramatically increases the risk of atherosclerotic cardiovascular disease (, ) and the reduction of atherogenic lipids could greatly reduce the mortality and morbidity of cardiovascular diseases in individuals with type 2 diabetes. The aim of this study was to investigate the safety and effectiveness of the psyllium shell fiber consumed by 8 k in conjunction with a standard diet for diabetes in the treatment of men with type 2 diabetes and mild to moderate hypercholesterolemia. The effects of psyllium on glucemic and serum lipid indices were examined in an outpatient and metabolic environment. SUBJECTS AND METHODS A total of 56 men with type 2 diabetes and hypercholesterolemia were initially recruited. After a dietary stabilization phase of 2 kwk, 34 of these men qualified for random assignment to treatment. The Human Research Subcommittee of the University of Kentucky reviewed and approved the study and obtained the informed consent of each topic. People were eligible for the study if they were men between 30 and 70 years old; they had a body mass index (in kg/m2) of ≤30; they had a stable type 2 diabetes history that met the criteria of the national diabetes data group (Hb≤1c) with a blood glucose concentration of 8,33 to 11,10 mmol/L and a serum hemoglobin (Hb≤ol) Individuals whose diabetes was controlled by diet alone or diet plus oral sulfonymatolurea agents were eligible for study. People were excluded from the study if they had medical conditions or were taking medications or supplements that might have interfered with glucose, insulin or lipid measurements. Individuals with a history of myocardial infarction or major surgical procedures within the previous 6 mos were excluded from the study, such as individuals with a history of alcohol abuse, aspartame allergy or psyllium seed, or phenylcetonuria. Experimental design This study was double-blind, placebo-controlled and parallel. The study consisted of a phase of dietary stabilization of 2 kwk during which the subjects followed a diet for diabetes followed by an 8 kwk treatment phase in which the subjects continued the diet, but were also randomly assigned to receive a 5.1 g (Psilio group) or cellulose placebo (control group) twice a day. The subjects were instructed to consume test products 20–30 min before morning and evening meals. All subjects were subject to 2-d metabolic district studies at weeks 0 and 8. During these studies, standardized meals were used to measure more accurately the effects of psyllium on glucemic and lipid control. After an infusion of night insulin, a random subset of 8 subjects in the psyllium group and 8 subjects in the placebo group experienced an euglycemic clamping procedure during the third day of each metabolic evaluation of the pavilion to more fully assess the metabolism of glucose and the sensitivity of peripheral insulin. Diets and Test Products During the dietary stabilization phase, subjects received instruction on a traditional diet of exchange of weight diabetes that provides ≤30% total energy such as fat, ≤10% of energy as saturated fat, and ≥55% of energy as carbohydrate. The diet was not the main focus of this intervention and the main objective of dietary instruction was to encourage subjects to maintain their same dietary patterns throughout the study. The subjects continued this diet and received ongoing dietary advice throughout the rest of the study. During the treatment phase, the subjects of the psyllium group received a product without sugar and orange flavor (Metamucil; Procter & Gamble Co, Cincinnati); the subjects of the placebo group received insoluble fiber, microcrystalline cellulose (Avicel, PH-101; FMC Corp, Philadelphia). Both test products included the same excipients of psyllium product and were given in two doses of 8.7 g per day; each dose provided 5.1 g of psyllium or cellulose. Both products were orange-flavored powders and were packaged in identical aluminium packages. The subjects were instructed to mix each pack in 240 mL liquid and to drink the mixture immediately before (20–30 min) the morning and evening meals every day for 8 wk. During the metabolic room evaluations, subjects received low standardized fiber meals to improve the detection of fiber effects in glucose and lipid metabolism, as described above (). Subjects consumed a low-fat, low-consumption (65 per cent of energy such as carbohydrate, 15 per cent as protein, 20 per cent as fat, and 50 mg of cholesterol/MJ) on the night of the first day of the evaluation of the metabolic room. On Day 2 of the metabolic evaluation, subjects consumed 3 meals that provided 40% of energy as carbohydrate, 15% as protein, 45% as fat, 50 mg of cholesterol/MJ, and 0.8 g of dietary fiber/kJ. Dietary compliance throughout the study was monitored through the use of 3D food records collected in weeks −1, 4 and 8. Dietary data for energy, total fat, polyunsaturated fat, saturated fat, carbohydrates, proteins, total fiber, soluble fiber, and cholesterol content were analyzed using a computed nutrient database () with revised fiber values (). Compliance with the use of the test product was supervised by subject interviews and counting unopen packages on follow-up visits. Reports of any negative treatment-related experience were requested on each follow-up visit. A short physical examination, a full lipid profile and fast blood glucose and blood glucose concentrations of hemoglobin glucose glucose glucose glucose glucose glucose glucose (Hb A1c) were performed at a week −2 to establish eligibility for the study and were repeated in weeks −1, 0, 2, 4, 6, and 8. Concentrations of fasting albumin glucose were measured in weeks −1, 0, 2, 4, 6, and 8 of the study. Thyroid function tests were also measured at −1 week of the study. Clinical visits were scheduled in the morning after a minimum of 12 h fast. Subjects were ordered not to take their test medication in the morning of study visits. At weeks 0 and 8, all subjects were admitted to the metabolic pavilion for 2-3 d of evaluation. A complete physical examination, routine clinical chemistry and hematological evaluations, and urine was performed on day 1. The serum fasting lipid, the C peptides, Hb A1c and the glucogram albumin concentrations were some of the measured indices. On the 2nd day of the metabolic evaluation of the room, the lipids serum, glucose, insulin, fatty acids, apolipoproteins and lipoprotein fractions by a vertical auto profile (VAP) were measured immediately before breakfast after a 14h fast. Postprandial lipids, glucose and insulin concentrations were measured at 9 intervals throughout the day; postprandial fatty acids were measured at 7 intervals; and postprandial apolipoproteins and VAP lipoproteins were measured at 3 intervals. A catheter was inserted into an antecubital vein to limit the number of venipunctures. On the morning of day 3 of the evaluation of the metabolic room, 16 randomly selected subjects were also subjected to a procedure of eugenic hyperinsulinemic clamping (, ). In order to standardize the basal concentrations of serum glucose, the subjects received an insulin infusion during the night (W Duckworth, unprecedented observations, 1992). Briefly, a 12 h intravenous insulin infusion (Novolin R in 1 l isotonic saline; Squibb & Co, Princeton, NJ) started on these issues on the night of day 2. The insulin delivery rate was started and adjusted per hour according to a predetermined algorithm based on blood glucose. Insulin was infused in ♥1 mU•kg−1•min−1 for 3 h after a proper dose of pricing. Glucose (20% wt:vol, or 1.1 mol/L) was infused to keep glucose in the blood at 5.55 mmol/L. The blood was extracted every 5 min along the procedure to monitor blood glucose concentrations, and 6 serum insulin evaluations were performed at regular intervals during the procedure. The subjects who were subjected to the euglycemic clamp were released after postclamp food. All other subjects were discharged after breakfast on day 3. Analytical methods Serum glucose concentrations were measured by oxidase glucose (). Serum insulin concentrations were measured with a radioinsulin kit (ICN Micromedic Systems, Horsham, PA). Serum, triacylglycerol and HDL-choesterol cholesterol levels were determined by enzyme methods using VP Abbott (Abbott Laboratories, North Chicago). Serum cholesterol concentrations were measured with an ester-cholesterol oxidase test (). Serum triacilglicerol concentrations were determined by hydrolysing triacilglicerol and measuring the released glycerol (). The concentrations of HDL-cholesterol cholesterol were measured with the same method used for serum cholesterol after the elimination of LDL and VLDL cholesterol by precipitation of magnesium-dextran sulfate (). Apolipoprotein A-I and B-100 concentrations were measured by radioimmundifusion with Tago-Diffu-Gen kits (Tago, Burlingame, CA). Samples were sent to the University of Alabama Lipoprotein Laboratory (Birmingham) for VAP measurements (). Other lipid measurements were performed locally. Serum LDL-cholesterol, intermediate-density-lipoprotein (IDL), VLDL-cholesterol, HDL2, and HDL3 concentrations were available from the VAP analysis. LDL cholesterol was also calculated with the Friedewald formula (). C-peptide serum concentrations were measured as described above (). The albumin Glycated was measured using a column of boroned affinity (Nichols Institute Reference Laboratories, San Juan Capistrano, CA), with expected values of 0.9–1.9%. Statistical Analysis Two sampling tests confirmed by Wilcoxon rank-sum were used to determine the comparability of the values for the psyllium and placebo groups on the basis, to compare percentage changes and changes in the baseline between the treatment groups, and to compare dietary analysis rates between groups. Tests of a t-sample were used to determine whether the average baseline changes in each treatment group were significant. For the final values of body weight and each of the glucemic and lipid profile indices, covariance analysis was also completed with reference values such as covariates. For outpatient evaluations, reference values are defined as the average of all values taken in weeks −2, −1, and 0. The final values are defined as the measured at week 8. For metabolic evaluations, base and end values were defined as an average of values taken on the 2nd day of the assessment of metabolic districts at weeks 0 and 8, respectively. The measured values during the euglycemic clamping procedure were analyzed separately from other metabolic vertrum assessments. The glucose and insulin values of the medium and peak serum were calculated separately for postprandial periods after breakfast, lunch and dinner. All topics were included in the security analysis, while only subjects who meet all the inclusion and exclusion criteria were included in the effectiveness analysis. RESULTS of P values of two tailsOf the 56 men who entered the phase of dietary stabilization, 19 did not meet the criteria of inclusion and exclusion of the study and 3 removed their consent to participate. Of the 34 subjects randomly assigned to treatment (18 to the psyllium group and 16 to the placebo group), 29 (15 in the psyllium group and 14 in the placebo group) completed the study and were considered to be evaluable. In the psyllium group, a subject withdrew consent, a subject was discharged by the study investigator due to back pain due to a non-treatment-related spinal infection, and a subject was considered unevaluable due to a blood glucose concentration of basal fasting in violation of the study protocol. In the placebo group, a subject withdrew consent and a subject was discharged by the study investigator due to non-compliance. On the basis of the number of returned packages, without opening and subject interviews, it was determined that compliance was excellent. Subjects consumed 99.6% of the psyche and 95.3% of the given placebo. Basal Characteristics The baseline characteristics of the subjects in the psyllium and placebo groups are summarized in . Subjects were well adjusted according to age, height, body weight and body mass index. Concentrations of C basal peptides were not significantly different between groups. Baseline Characteristics of Subjects in Psychology and Variable Control Groups . Control (n = 14) . Psyllium (n = 15) . Age (y) 63.8 ± 1.6 62.0 ± 1.6 Height (cm) 178.6 ± 2.0 176.8 ± 1.4 Body weight (kg) 87.1 ± 3.3 89.6 ± 2.4 Body mass index (kg/m2) 27.4 ± 1.1 28.7 ± 0.9 C-peptide (nmol/L) 1.16 ± 0.10 1.32 . Control (n = 14) . Psyllium (n = 15) . Age (y) 63.8 ± 1.6 62.0 ± 1.6 Height (cm) 178.6 ± 2.0 176.8 ± 1.4 Body weight (kg) 87.1 ± 3.3 89.6 ± 2.4 Body mass index (kg/m2) 27.4 ± 1.1 28.7 ± 0.9 C-peptide (nmol/L) 1.16 ± 0.10 1.32 ± 0.10 There were no significant differences between groups. Baseline Characteristics of Subjects in Psychology and Variable Control Groups . Control (n = 14) . Psyllium (n = 15) . Age (y) 63.8 ± 1.6 62.0 ± 1.6 Height (cm) 178.6 ± 2.0 176.8 ± 1.4 Body weight (kg) 87.1 ± 3.3 89.6 ± 2.4 Body mass index (kg/m2) 27.4 ± 1.1 28.7 ± 0.9 C-peptide (nmol/L) 1.16 ± 0.10 1.32 . Control (n = 14) . Psyllium (n = 15) . Age (y) 63.8 ± 1.6 62.0 ± 1.6 Height (cm) 178.6 ± 2.0 176.8 ± 1.4 Body weight (kg) 87.1 ± 3.3 89.6 ± 2.4 Body mass index (kg/m2) 27.4 ± 1.1 28.7 ± 0.9 C-peptide (nmol/L) 1.16 ± 0.10 1.32 ± 0.10 There were no significant differences between groups. The dietary nutrient intakes and basis in the psyllium and placebo groups are shown in . Except for the significantly higher total energy intake in the psyllium group than in the placebo group at the base, dietary intakes do not differ significantly between groups throughout the study. The scant energy shots reported by the psyllium and placebo groups in this study indicated that the subjects substantially underestimated their food consumption. More intensive training of subjects is required to ensure accurate self-reported intake for careful dietary studies. Daily nutrient intakes of subjects in psycholithic and control groups . Control (n = 14) . Psyllium (n = 15) . Nutrients . Baseline . Final . Baseline . Final ± 32.9 ± 1.6 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± , ± ± ± , ± ± ± ± ± , ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± . . . . . . . . . . . . . . . . . . . . . . . Control (n = 14) . Psyllium (n = 15) . Nutrients . Baseline . Final . Baseline . Final ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.6 ± 2.6 ± ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 Baseline and end values were measured in weeks 1 and 8, respectively. Significantly different from the control group,P Polyunsaturated fat ratio to saturated fat. Daily nutrient intakes of subjects in psycholithic and control groups . Control (n = 14) . Psyllium (n = 15) . Nutrients . Baseline . Final . Baseline . Final ± 32.9 ± 1.6 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± , ± ± ± , ± ± ± ± ± , ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± ± . . . . . . . . . . . . . . . . . . . . . . . Control (n = 14) . Psyllium (n = 15) . Nutrients . Baseline . Final . Baseline . Final ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.6 ± 2.6 ± ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 ± 2.0 Baseline and end values were measured in weeks 1 and 8, respectively. Significantly different from the control group,P Polyunsaturated fat ratio to saturated fat. Outpatient Responses The base changes in the glucemic and lipid indices of the 2 groups during the outpatient and metobolic parts of the study are summarized in . Week 8, the concentrations of serum LDL-cholesterol decreased 4.9% in the psycholithic group, but increased 2.8% in the placebo group. This difference of 7.7% in serum concentrations of LDL-cholesterol was almost significant (P = .09). The change in serum concentrations HDL-cholesterol was significantly different between psyllium and placebo groups at week 8, although the change in the relationship of LDL to HDL cholesterol was significantly different. Apart from these exceptions, there were no significant differences in the change in glucemic and lipid indices between psyllium and placebo groups during outpatient evaluations. Glucemic and lipid responses serum in metabolic and outpatient rooms in psyche and control groups . Control (n = 14) . Psyllium (n = 15) . . Baseline . Percentage change . Baseline . Percentage change . 0.2 ± 3.0 ± 3.0 ± 3.0 ± 3.0 ± 3.0 ± 3.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.00.0 . Control (n = 14) . Psyllium (n = 15) . . Baseline . Percentage change . Baseline . Percentage change . 0.2± 3.0± 3.0± 3.00.0 Reference values were measured in weeks −2, −1, and 0; end values were measured in week 8. VAP, auto verticle profile; Hb A1C, hemoglobin glucose. Significantly different from control group: P Significantly different from control group: P = 0.01.Serum glycemic and lipid responses in metabolic ward and outpatient settings in subjects in the psyllium and control groups . Control (n = 14) . Psyllium (n = 15) . . Baseline . Percentage change . Baseline . Percentage change . 0.2 ± 3.0 ± 3.0 ± 3.0 ± 3.0 ± 3.0 ± 3.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.2 ± 0.00.0 . Control (n = 14) . Psyllium (n = 15) . . Baseline . Percentage change . Baseline . Percentage change . 0.2± 3.0± 3.0± 3.00.0 Reference values were measured in weeks −2, −1, and 0; end values were measured in week 8. VAP, auto verticle profile; Hb A1C, hemoglobin glucose. Significantly different from the control group: P significantly different from the control group: P = 0.01.All subjects maintained their body weights within ±5% during the study. As shown in , body weight decreased 0.3% in the psycholithic group but increased 1.5% in the placebo group to week 8. Although this 1.8% difference in body weight change between psyllium and placebo groups was significant by week 8, there were no consistent trends in body weight during the study. Changes in body weights do not differ significantly between groups at weeks 2, 4 or 6.Answers to the metabolic room The base changes in the serum glucose with treatment are illustrated in . During the first 180 min of treatment, the values for subjects of the placebo group do not differ significantly from the base, but the values were consistently higher than the baseline to 270 min and beyond, being significantly different to 420 and 480 min. On the contrary, the values of the subjects treated with psyllium were constantly below the reference values and differed significantly from the values of the placebo group in 420 and 480 min. Average changes (±SEM) (ends to week 8 - starting values per week 0). in serum glucose concentrations before and after meals for subjects in placebo (♦) and psyllium (▪). * Significant difference between groups, P Mean (±SEM) changes (ends to week 8 - initial values to week 0). in serum glucose concentrations before and after meals for subjects in placebo (♦) and psyllium (▪). * Significant difference between groups, P Changes from the baseline in glucemic and lipid indices during metabolic room evaluations and external patients are also shown in . There were significant differences in base changes between the 2 groups for glucemic and lipidal indices, with the psyllium group that showed better metabolic control compared to placebo group subjects. Of the Glycemic indices measured in all subjects in the metabolic pavilion, the percentage change in postprandial serum glucose concentrations of all days and postlunched serum glucose concentrations differ significantly between psyllium and placebo groups. Compared to base concentrations, postprandial serum postprandial glucose concentrations all day decreased 4.2 per cent in the psyllium group, but increased 6.8% in the placebo group (Glucemic indexes measured during insulin clamping studies were not significantly different before and after treatment in psyllium and placebo groups. After an infusion of night insulin, the base serum glucose values averaged 7.6 ± 0.6 and 7.5 ± 0.5 mmol/L in the psyllium and placebo groups, respectively; these values do not differ significantly between groups after the treatment period of 8 kwk. The mean concentrations of serum glucose during the reference insulin clamping procedure were 6.2 ± 0.1 and 6.1 ± 0.2 mmol/L in the psyllium and placebo groups, respectively; these values do not differ significantly between groups after treatment. The mean concentrations of serum insulin during the basal insulin clamping procedure were 517.4 ± 17.4 pmol/L (74,5 ± 2.7 mU/mL) and 470.2 ± 38.9 pmol/L (67.7 ± 5.6 mU/mL) in the psyche and control groups, respectively; these values did not vary significantly after treatment. Glucose infusions during the reference insulin clamping procedure averaged 2.3 ± 0.7 and 2.4 ± 0.5 mg•kg−1•min−1 in psyche and control groups respectively; these values decreased by 4.4 ± 5.3% and 4.2 ± 13.8%, respectively, during treatment. Therefore, there were no significant differences in these glucemic indices or the percentage changes in these indices between psyllium and control groups at the base or after treatment. Of the lipid indexes measured in the metabolic pavilion, the percentage changes in the total concentrations of serum cholesterol differ significantly between psyllium and placebo groups (P = 0.012). Differences in percentage changes between groups were almost significant for calculated LDL cholesterol concentrations (P = 0.068) and LDL-VAP cholesterol concentrations (P = 0.068). Total concentrations of serum cholesterol decreased 2.1% of the base in the psycholithic group, but increased 6.9% in the placebo group, resulting in a net difference in total concentrations of serum cholesterol of 9.0% among the 2 groups. Security Analysis Security analysis was performed in the 34 subjects assigned to random treatment. Most of the subjects well tolerated test products. There were no significant differences between treatment groups in the incidence of adverse events or the type of event reported. Respiratory system disorders were the most commonly reported adverse events. The placebo or psyllium group did not report serious adverse events related to treatment. Except for the increase in total concentrations of proteins and γ-glutamyltransferase and significant changes in some of the indices of leucocytes in the placebo group compared to the baseline, there were no clinically significant changes in clinical chemistry, hematology or orinalosis rates as a result of treatment in both groups. Although the difference in base changes between psyllium and placebo groups was significant for total protein, γ-glutamyltransferase concentrations, and some leukocyte indices, none of these indices significantly changed from the baseline in the psyllium group. DISCUSSION This study was designed to assess the safety and effectiveness of the psyllium compared to a placebo of cellulose used in conjunction with a traditional diet of diabetes in men with type 2 diabetes and mild to moderate hypercholesterolemia. Significant differences were observed in the baseline changes between treatment groups in both Glycemic and lipid indexes evaluated in the metabolic pavilion, with the psyllium group showing better metabolic control compared to the placebo group. Although most changes in glucemic and lipid indices during outpatient evaluations were not significantly different from treatment groups, directional changes also suggested improving metabolic control in the psyllium group. The magnitude of the total serum and the reductions of the LDL-colesterol observed in this study were similar to the reductions reported in studies of non-diabetic individuals. Sprecher et al () reported significant net decreases (small placebo psyllium) in total and LDL cholesterol-concentration of 3.5% and 5.1%, respectively, after 8 psyllium treatment wk (5.1 g twice a day) in subjects who consume a low fat diet. In a similar study with a dietary stabilization phase of 8 kwk, Bell et al () reported significant net decreases in total concentrations and LDL-cholesterol of 4.8% and 8.2%, respectively, after the supplementation of psyllium and placebo. In large-scale studies of non-diabetic people with hypercholesterolemia, 8-16 psyllium treatment wk after a dietary stabilization phase reduced total concentrations of serum cholesterol by 3.5-5.6% and serum concentrations of LDL-cholesterol by 5.1-8.8% compared to placebo treatment (, –). This smaller-scale study may not have had enough statistical power to detect all the significant effects of psychal treatment. Additional large-scale studies are required to confirm the preliminary results of this study. Previous studies reported that psyllium reduced serum fasting glucose concentrations () or decreased postprandial serum glucose concentrations () in individuals with type 2 diabetes. In another study, the psyllium reduced the glycemic response of diabetic people to a meal of bran cereals flashed only when the psyllium was incorporated or sprayed on the cereal (). In a carefully controlled cross-sectional study of the psyllium effects taken immediately before breakfast and dinner compared to the effects of placebo cellulose supplementation in individuals with type 2 diabetes, postprandial serum glucose values were 14% lower after breakfast, 31% lower after lunch, and 20% lower after dinner with psyllium (). The capacity of soluble fibers to reduce the response of postprandial glucose to meals that are eaten several hours after the ingestion of fiber (e.g., the so-called second effect of food) was previously shown in non-diabetic individuals (, ).The side effect of the psyllium was also evident in the present study. Two doses of psyllium taken immediately prior to breakfast and dinner resulted in significantly lower measurements of postprandial glucose all day and postlunch serum glucose concentrations in the psyllium than in the placebo group. Concentrations of postprandial glucose all day and postlunch were 11.0% and 19.2% lower, respectively, in the psyche than in the placebo group. It is unlikely that constant improvements in metabolic indices seen in the psyllium group in this study were due to weight changes. Although the body weights were 1.8% lower in the psycholithic group than in the placebo group at week 8 (P Except for the highest intakes of energy in the psycholithic group at the base, the dietary intakes were not significantly different between the groups during the study. The low energy consumption reported by both groups indicated that the subjects submitted to their food consumption, as documented in other clinical studies (). The present study did not aim to be a careful dietary study, but rather the purpose of dietary instruction and monitoring in this study was to ensure that dietary intake did not change significantly and that there were no significant differences in dietary intake between treatment groups during the study. Careful dietary studies require intensive instruction and monitoring beyond the scope of this study. The plill is a viscose water soluble fiber that has been used for a long time as bulk laxative with a good safety record. Although the role of dietary fiber in nutritional therapy for type 2 diabetes remains controversial (, ), several studies indicate that high-content (–) or diets supplemented by soluble fibers such as guar (), soy (), or pectin () improve metabolic control in many individuals with type 2 diabetes. Practical applications for some soluble fiber sources, however, are limited due to the lack of palatable shapes. In this study, the psyllium was well tolerated, associated without serious adverse events, and improved metabolic control compared to a cellulose placebo. Medical nutrition therapy in type 2 diabetes should be individualized to reflect the personal goals of lifestyle and management (). Because type 2 diabetes significantly increases the risk of atherosclerosis and its complications (), achieving and maintaining normal concentrations of serum lipids is a primary goal of managing diabetes that could greatly reduce death and disability in this population. The results of this study suggest that the addition of psyllium to a standard diabetes diet is safe, well tolerated and offers an additional dietary tool to improve metabolic control in individuals with type 2 diabetes and hypercholesterolemia. We recognize Nancy J Gustafson's expert technical writing skills and Heather A Tully's statistical experience. PHOOTNOTESAported by The Procter & Gamble Co, Cincinnati. Email Alerts More About This Subject Related Articles in Related Articles in PubMedCiting ConnectResources ExploreOxford University Press is a department at Oxford University. In addition, the University's goal of excellence in research, scholarship and education by publishing around the world or This PDF is available for Subscribers OnlyFor full access to this pdf, enter an existing account or purchase an annual subscription.

Metamucil Sugar Free Orange Smooth Fiber Powder | Metamucil®

Know How Psyllium Fiber Helps Maintain Blood Sugar Levels | Metamucil
Is Metamucil Safe? The Truth Behind This "Doctor Recommended" Product

Benefiber vs. Metamucil: Which Is Better for Me?
:max_bytes(150000):strip_icc()/the-benefits-of-psyllium-89068-dddeb2ed5bb24522b5ae656ef89f717c.png)
Psyllium: Benefits, Side Effects, Dosage, and Interactions

Metamucil Powder with No Added Sweetener | Metamucil

Metamucil 3-in-1 Psyllium Fiber Supplement Capsule, 160 ct - Walmart.com - Walmart.com

Metamucil and Cholesterol: Is There a Connection?

Liz, Author at Lizs Healthy Table - Page 21 of 54
Know How Psyllium Fiber Helps Maintain Blood Sugar Levels | Metamucil
Is Metamucil Safe? The Truth Behind This "Doctor Recommended" Product

Amazon.com: Metamucil Premium Blend, Natural Psyllium Husk Powder Fiber Supplement, Plant Based, Sugar-Free with Stevia, 4-in-1 Fiber for Digestive Health, Orange Flavored, 180 teaspoons (36.5 OZ Fiber Powder): Health & Personal Care

Organic Metamucil: Best Natural Products

Know How Psyllium Fiber Helps Maintain Blood Sugar Levels | Metamucil

Benefiber vs. Metamucil: Differences, similarities, and which is better for you

Two-week Challenge: To Stay Regular & Avoid Constipation | Metamucil

Metamucil for Weight Loss: Should You Try It?
Is Metamucil Keto Friendly? | Is It Keto

Benefiber vs Metamucil: Benefits, side effects, and dosage

Can Dogs Take Metamucil For Constipation? | Is It Safe?

Know How Psyllium Fiber Helps Maintain Blood Sugar Levels | Metamucil

Know How Psyllium Fiber Helps Maintain Blood Sugar Levels | Metamucil

Psyllium fiber: Regularity and healthier lipid levels? - Harvard Health

Metamucil Sugar-Free Orange Powder Packets Box

Metamucil Weight Loss Fiber - WeightLossLook

Take the Two-Week Metamucil Challenge to Boost Your Daily Fiber Intake
Is Metamucil good or bad for tye 2 ? - Type 2 Diabetes - Diabetes forums

Metamucil 3 in 1 MultiHealth Fibre! Sugar-Free Fiber Suplement Powder Packets, Orange, 44 x 5.8 g (Packaging may vary): Amazon.ca: Health & Personal Care

Know How Psyllium Fiber Helps Maintain Blood Sugar Levels | Metamucil

Metamucil Psyllium Stevia Fiber Supplement Powder, Orange, 114 Tsp - Walmart.com - Walmart.com

Does Metamucil Lower LDL Cholesterol? | Answers From Pritikin Experts

Metamucil 14-Day Cleanse Fiber, Eliminate Waste, 30 Servings, Psyllium Husk Fiber Supplement, Sugar-Free Powder,

4 Best Fiber Supplements

METAMUCIL FIBER, 4-IN-1 PSYLLIUM FIBER SUPPLEMENT, SUGAR-FREE POWDER, ORANGE FLAVORED DRINK - CVS Pharmacy

How to Maintain Healthy Blood Sugar Levels & Increase Fiber Intake with Metamucil - YouTube
Metamucil 3 in 1 MultiHealth Fibre Suplement Power Sugar-Free, 228 Doses
Take the Two-Week Metamucil Challenge to Boost Your Daily Fiber Intake

Is Metamucil Good For Diabetics | DiabetesTalk.Net

Benefiber vs Metamucil: Benefits, side effects, and dosage

Metamucil Psyllium Husk Fiber
Posting Komentar untuk "is metamucil good for diabetics"